Regenerative Medicine News and General Information
New Way to Eradicate Bacterial Infection
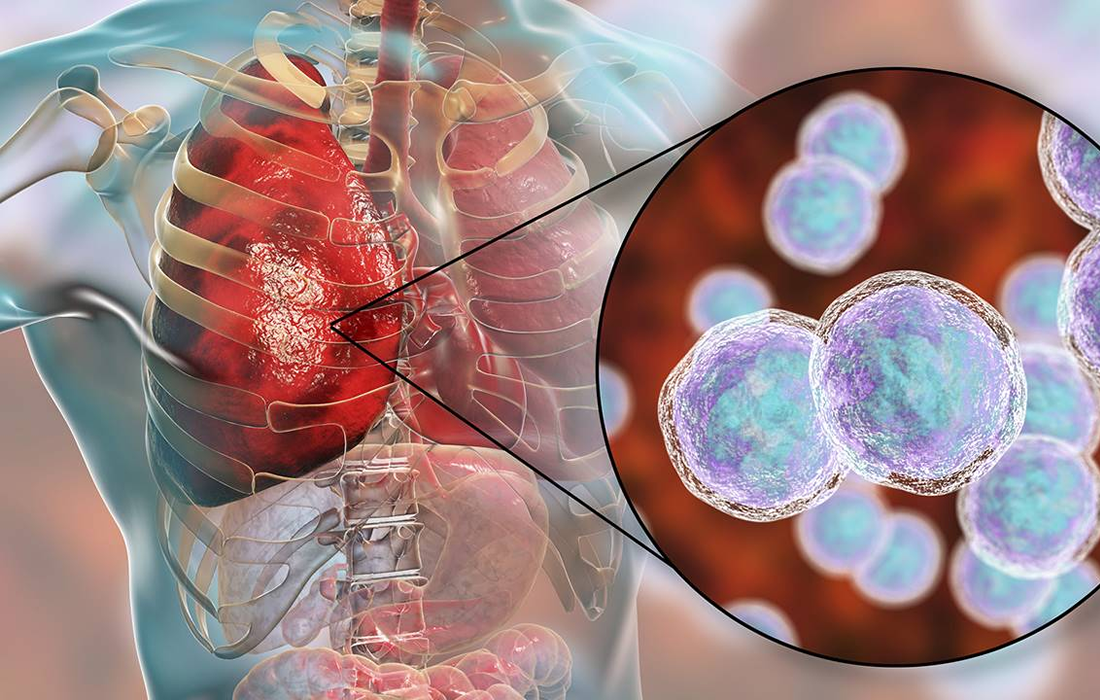
Community-acquired pneumonia (CAP) is one of the most common infectious diseases addressed by clinicians and is an important cause of mortality and morbidity worldwide.
Typical bacterial pathogens that cause CAP include S pneumoniae, H influenzae, and M catarrhalis. Numerous other organisms can cause CAP in the appropriate clinical setting.
Furthermore, the so-called “atypical CAP” pathogens are actually common causes of CAP and were originally classified as atypical because they are not readily detectable on Gram stain or cultivable on standard bacteriological media.
CAP is usually acquired via inhalation or aspiration of a pathogenic organism.
Epidemiology of Community-Acquired Pneumonia
The incidence of CAP varies greatly from country to country. In the United States, CAP is estimated to occur in 248 of 10,000 adults annually, whereas a study from the Veterans Health Administration noted 472.2 cases per 100,000 person-years in 2017.
Patient History
Patients with community-acquired pneumonia (CAP) due to typical bacterial CAP pathogens commonly present with fever, dyspnea, and productive cough, often with pleuritic chest pain.
The clinical presentation of atypical CAP is more subacute and associated with extrapulmonary manifestations that may provide a clue to the etiology.
Physical Examination
Purulent sputum is characteristic of pneumonia caused by typical bacterial community-acquired pneumonia (CAP) pathogens and is not usually a feature of pneumonia caused by atypical pathogens, with the exception of Legionnaires disease. Blood-tinged sputum may be found in patients with pneumococcal pneumonia, Klebsiella pneumonia, or Legionella pneumonia.
Rales are heard over the involved lobe or segment. Consolidation may be accompanied by an increase in tactile fremitus, bronchial breath sounds, and egophony.
Treatment
Preferred monotherapy for mild or outpatient CAP includes a macrolide, amoxicillin, or doxycycline. For patients with an increased risk for resistance or with numerous comorbidities, monotherapy options include respiratory quinolone. Prior to the use of a fluoroquinolone, an assessment of contraindications and risk of adverse effects should be performed.
Mild to moderately ill patients with CAP may be treated entirely via the oral route, on either an inpatient or outpatient basis. Patients who are severely ill or unable to tolerate or absorb oral medications require some duration of intravenous therapy before switching to an oral antibiotic.
The duration of therapy for uncomplicated CAP is usually 5 days.
New possible way to treat these infections
Nanoengineers at the University of California San Diego have developed microscopic robots, called microrobots, that can swim around in the lungs, deliver medication and be used to clear up life-threatening cases of bacterial pneumonia.
In mice, the microrobots safely eliminated pneumonia-causing bacteria in the lungs and resulted in 100% survival. By contrast, untreated mice all died within three days after infection.
The team used the microrobots to treat mice with an acute and potentially fatal form of pneumonia caused by the bacteria Pseudomonas aeruginosa. This form of pneumonia commonly affects patients who receive mechanical ventilation in the intensive care unit. The researchers administered the microrobots to the lungs of the mice through a tube inserted in the windpipe. The infections fully cleared up after one week. All mice treated with the microrobots survived past 30 days, while untreated mice died within three days.
Treatment with the microrobots was also more effective than an IV injection of antibiotics into the bloodstream. The latter required a dose of antibiotics that was 3000 times higher than that used in the microrobots to achieve the same effect.
These results show how targeted drug delivery combined with active movement from the microalgae improves therapeutic efficacy
AS we can see, there is a possibly way to deliver medication direct on the lungs and maintain the effect to treat better pneumonia infections, especially the intrahospitalize infections such as P. aeruginosa, it is a bacterial infection difficult to eradicate because of the antibiotic resistance that has been developing in the last few years. Larger studies and human studies are needed in the future.
SOURCE:
Fangyu Zhang, Jia Zhuang, Zhengxing Li, Hua Gong, Berta Esteban-Fernández de Ávila, Yaou Duan, Qiangzhe Zhang, Jiarong Zhou, Lu Yin, Emil Karshalev, Weiwei Gao, Victor Nizet, Ronnie H. Fang, Liangfang Zhang, Joseph Wang, (September 22, 2022). Nanoparticle-modified microrobots for in vivo antibiotic delivery to treat acute bacterial pneumonia. Nature Materials. Retrieved from : https://www.nature.com/articles/s41563-022-01360-9
https://emedicine.medscape.com/article/234240-overview#a1
IMAGE:
https://content21.sabervivirtv.com/medio/2021/01/11/neumonia-ficha_f1171fba_1280x720.jpg

